Introduction to Oral and Maxillofacial Surgery
Oral and maxillofacial surgery is a specialized field of dentistry that focuses on diagnosing and treating conditions affecting the mouth, jaws, and face. This branch of surgery is essential in addressing a variety of issues, including facial trauma, congenital deformities, and complex dental diseases. Surgeons within this discipline possess a unique skill set that combines both dental and medical training, allowing them to deliver comprehensive care tailored to each patient’s needs.
The scope of oral and maxillofacial surgery encompasses numerous procedures, ranging from simple tooth extractions to highly complex surgeries such as jaw reconstruction and facial implants. Additionally, these surgeons perform treatments for various pathological conditions, including cysts and tumors of the oral cavity and jaws. They also address cosmetic concerns, such as orthognathic surgery aimed at correcting jaw alignment, thus improving both function and appearance.
One of the notable aspects of oral and maxillofacial surgery is its critical role in overall health. Oral health is closely linked to systemic health, with research indicating that dental infections can contribute to various medical conditions. This highlights the importance of procedures performed by oral and maxillofacial surgeons in preventing and managing infections, thereby safeguarding patients’ overall health. Furthermore, these specialists work in collaboration with other healthcare providers, ensuring a multidisciplinary approach to treatment that enhances patient outcomes.
As we delve deeper into the realm of oral and maxillofacial surgery, it becomes evident that this specialty is vital not only for addressing dental issues but also for impacting patients’ overall well-being. Understanding its significance lays the groundwork for exploring the specific procedures and advancements associated with this essential surgical field.
Common Procedures in Oral and Maxillofacial Surgery
Oral and maxillofacial surgery encompasses a range of surgical procedures aimed at diagnosing and treating conditions related to the mouth, jaws, and face. Among the most common procedures performed in this specialty are wisdom tooth extraction, corrective jaw surgery, facial trauma repair, and the management of oral cancers. Each of these interventions serves significant purposes in enhancing oral health and restoring functionality.
Wisdom tooth extraction is arguably one of the most familiar procedures in the field. This operation is typically indicated when wisdom teeth become impacted, meaning they do not fully emerge from the gums. Impacted wisdom teeth can lead to pain, infection, and misalignment of surrounding teeth. By surgically removing these teeth, patients can alleviate discomfort and prevent further dental complications.
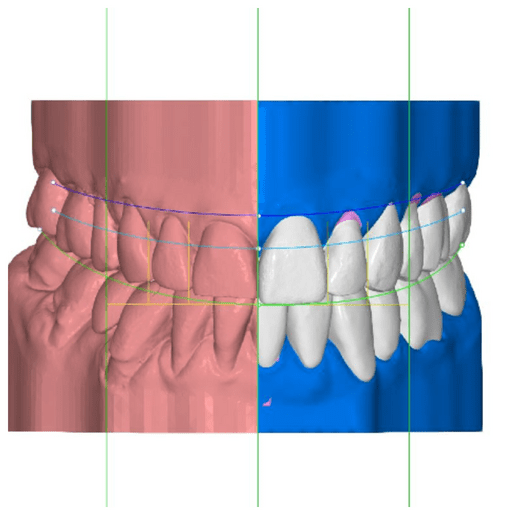
Corrective jaw surgery, also known as orthognathic surgery, is another essential procedure that addresses skeletal and dental irregularities. This surgery corrects misalignments between the upper and lower jaws, which can severely impact a patient’s ability to chew, speak, and maintain proper oral health. By repositioning the jaw, this procedure helps improve both function and facial aesthetics.
Facial trauma repair is critical for individuals who have sustained injuries due to accidents or other incidents. This type of surgery is aimed at reconstructing facial structures, restoring normal function and appearance. Surgeons may use a combination of techniques to realign the bones, repair soft tissue, and address any associated dental injuries.
Lastly, the management of oral cancers involves the surgical removal of tumors within the oral cavity and surrounding areas. Early detection and intervention are crucial to increasing the chances of recovery. Surgeons work collaboratively with oncologists to create a comprehensive treatment plan tailored to each patient’s needs, ensuring optimal outcomes.
The Role of Oral and Maxillofacial Surgeons
Oral and maxillofacial surgeons are highly trained specialists who focus on diagnosing and treating conditions affecting the mouth, jaws, face, and neck. The path to becoming an oral and maxillofacial surgeon is rigorous and demands a commitment to extensive education and specialized training. Typically, aspirants begin their journey with a dental degree, which generally requires four years of undergraduate study followed by four years of dental school to earn either a Doctor of Dental Surgery (DDS) or Doctor of Medicine in Dentistry (DMD). This foundational knowledge in dentistry is crucial, as these professionals are uniquely qualified to understand complex oral anatomy and the implications of surgical interventions in this area.
Following their dental education, candidates must undergo a surgical residency program. These programs can span four to six years and include advanced training in surgical techniques, anesthesia, emergency medicine, and patient management. Residents gain hands-on experience through rotations in various medical settings, allowing them to collaborate with other healthcare professionals and broaden their skill set. The residency is particularly critical as oral and maxillofacial surgeons often manage challenging cases that require both dental and medical expertise, such as jaw deformities, facial trauma, and oral cancers.
Continuing education is another essential aspect of an oral and maxillofacial surgeon’s career. Given the constant advancements in medical technology and surgical techniques, staying updated with the latest research and innovations is paramount. Professional organizations provide valuable resources, including workshops and seminars that encourage practitioners to refine their skills. Furthermore, oral and maxillofacial surgeons frequently work within multidisciplinary teams, collaborating with orthodontists, ENT specialists, plastic surgeons, and primary care physicians. This teamwork not only enhances patient care but also reinforces the surgeon’s critical role in managing complex cases effectively.
Patient Experience: From Consultation to Recovery
Embarking on the journey of oral and maxillofacial surgery can be both exciting and intimidating for patients. Understanding what to expect during this process is essential for alleviating anxiety and fostering a sense of confidence. The first step in the patient experience is the initial consultation, where the oral and maxillofacial surgeon conducts a thorough examination, discusses medical history, and outlines the surgical options tailored to the patient’s needs.
During this consultation, patients can expect to learn about the specific procedure recommended, including risks, benefits, and anticipated outcomes. It is also an opportunity for patients to voice their concerns and ask questions regarding the surgery. This important dialogue helps establish a trusting relationship between the patient and the surgeon, ensuring that everyone is on the same page regarding treatment goals.
Once the decision for surgery is made, patients will delve into the surgical process itself. Prior to the procedure, various anesthesia options will be presented—from local anesthesia to sedation and general anesthesia—depending on the complexity of the surgery. Understanding these choices allows patients to feel more comfortable with their anesthesia plan and the overall surgical process.
Post-operative care is vital for a smooth recovery. Patients will receive detailed instructions on how to manage pain, swelling, and any potential complications. Follow-up appointments are essential to monitor healing and address any concerns. Having a clear understanding of what to expect during every phase of the oral and maxillofacial surgery process helps mitigate apprehensions and enables patients to approach their surgical experience with greater confidence.
In conclusion, navigating the patient journey in oral and maxillofacial surgery involves a sequence of well-defined steps—from consultation through to recovery. By being informed, patients can find reassurance and prepare adequately for their procedures, ultimately leading to a more favorable surgical outcome.
Technological Advancements in Oral and Maxillofacial Surgery
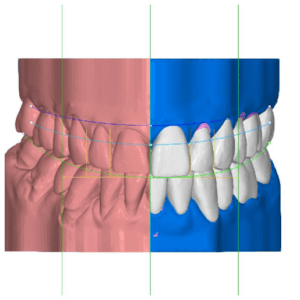
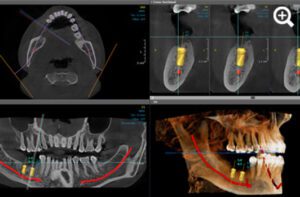
Oral and maxillofacial surgery has undergone significant transformations in recent years, largely driven by technological advancements that enhance surgical precision and improve patient outcomes. One of the most notable innovations is the advancement in imaging technologies. High-resolution imaging modalities such as cone beam computed tomography (CBCT) and three-dimensional (3D) imaging allow surgeons to visualize anatomical structures in unprecedented detail. This enhanced imaging capability facilitates improved preoperative planning, enabling more accurate diagnosis and treatment of complex cases, including jaw deformities and impacted teeth.
Another area of advancement is the development of minimally invasive surgical techniques. These techniques minimize tissue damage and reduce recovery times for patients. Techniques such as endoscopic surgery and laser-assisted procedures allow oral and maxillofacial surgeons to perform intricate operations through smaller incisions, which leads to less postoperative discomfort and a quicker return to normal activities. The reduction in recovery time not only enhances the patient experience but also contributes to lowering healthcare costs associated with longer hospital stays and postoperative care.
Furthermore, robotic-assisted surgery is revolutionizing the field. The incorporation of robotics in oral and maxillofacial procedures offers surgeons enhanced dexterity and control, resulting in greater precision during complex operations. Robotic systems can provide a stable platform that allows for fine movements that may be difficult to achieve with traditional surgical instruments. As a result, these systems significantly reduce the margin for error during procedures such as tumor resections and reconstructive surgeries.
Incorporating these technological advancements into oral and maxillofacial surgery not only improves outcomes for patients but also elevates the overall standard of care in the field. These innovations promise to continue evolving, paving the way for safer, more effective surgical interventions.
Challenges and Complications in Oral and Maxillofacial Surgery
Oral and maxillofacial surgery, while generally safe and effective, does carry certain challenges and complications that both patients and surgeons must consider. One primary concern involves the risks associated with anesthesia. Complications such as allergic reactions, respiratory difficulties, or even cardiovascular events can occur, underscoring the importance of thorough pre-operative assessments and discussions between the patient and the surgical team. Proper selection of anesthesia type and continuous monitoring during the procedure are critical in mitigating these risks.
Infection poses another significant challenge following surgery. The mouth contains a plethora of bacteria, and any surgical intervention can introduce pathogens into the bloodstream or surrounding tissues. It is essential for patients to adhere to post-operative care instructions to minimize infection risks. Surgeons often prescribe antibiotics or recommend antiseptic rinses to help protect against potential infections. Patients should be vigilant for symptoms such as increased swelling, fever, or unusual discharge, and report these to their healthcare provider promptly.
Nerve damage is another complication that can arise during oral and maxillofacial procedures. This may lead to sensations like numbness, tingling, or even chronic pain. Understanding the anatomy of the facial nerves is crucial for surgeons in order to avoid accidental injury. Patients should be made aware of this risk and encouraged to ask questions about nerve preservation techniques that may be utilized during their specific procedure.
Healing processes after surgery can vary significantly based on individual factors such as age, health status, and adherence to post-operative care. Communication between the patient and the surgeon remains essential to manage expectations, allowing patients to better understand their recovery timeline, potential complications, and any necessary lifestyle adjustments. Establishing a collaborative relationship can greatly enhance the overall surgical experience and outcomes for patients undergoing oral and maxillofacial surgery.
The Importance of Multidisciplinary Care
Oral and maxillofacial surgery is a specialized field that frequently intersects with various other medical disciplines, including orthodontics, otolaryngology, and oncology. This overlap necessitates a multidisciplinary approach to patient care, which has been increasingly recognized for its benefits in treating complex conditions. By collaborating across different specialties, healthcare providers can formulate comprehensive treatment plans that address all aspects of a patient’s health. This collaboration not only enhances the quality of care but also optimizes patient outcomes.
For instance, when addressing skeletal discrepancies or dental misalignments, oral and maxillofacial surgeons often work closely with orthodontists. This partnership ensures a thorough evaluation of the patient’s oral structure and assists in tailoring a treatment plan that accommodates both surgical and non-surgical interventions. By integrating orthodontic expertise in the planning stage, practitioners can minimize recovery time and enhance the effectiveness of the surgical outcomes.
Moreover, the intersection of oral and maxillofacial surgery and otolaryngology is vital in managing conditions such as obstructive sleep apnea or chronic sinusitis. Surgeons specializing in these areas must work together to ensure comprehensive care, considering potential airway complications that may arise during surgical procedures. This collaborative effort can significantly improve the patient’s overall health post-operation and enhance their recovery process.
In cancer treatment, the role of oral and maxillofacial surgeons is critical in the management of head and neck tumors. These specialists collaborate with medical oncologists and radiologists to devise treatment plans that encompass surgical removal of tumors, reconstruction, and rehabilitation. Incorporating insights from various fields allows for tailored interventions that address not just the tumor itself but also the long-term impacts of surgery on the patient’s quality of life.
In summary, the importance of a multidisciplinary approach in oral and maxillofacial surgery cannot be overstated. Collaborative care ensures that all relevant aspects of a patient’s health are considered, leading to more effective and personalized treatment plans. This approach enhances both the surgical outcomes and the overall healthcare experience for patients. Engaging various specialties in surgical planning highlights the value of comprehensive patient care, ultimately fostering better health results.
Future Trends in Oral and Maxillofacial Surgery
The field of oral and maxillofacial surgery is witnessing significant advancements driven by research initiatives, technological innovation, and evolving patient demographics. As we look to the future, a few key trends will be pivotal in shaping the landscape of this specialty. One notable development is the increasing application of minimally invasive techniques. Traditional surgical approaches often involve extensive incisions and prolonged recovery periods. However, innovations such as endoscopic surgery and robot-assisted procedures are gaining traction, which promise enhanced precision, reduced trauma, and improved patient outcomes.
Moreover, the integration of digital technology is poised to revolutionize surgical planning and execution. The use of 3D imaging and printing allows surgeons to create detailed anatomical models, facilitating more accurate preoperative planning. Furthermore, advancements in computer-assisted surgery are enabling real-time navigation during procedures, which enhances safety and efficiency. With augmented and virtual reality technologies emerging, today’s surgeons can practice complex procedures in a simulated environment, leading to improved skill acquisition and surgical confidence.
Another trend is the growing recognition of the importance of comprehensive patient care. As patient demographics change, with increasingly diverse populations presenting unique health challenges, oral and maxillofacial surgeons are adapting to address these needs more holistically. Multidisciplinary approaches that integrate specialists from various fields are becoming standard practice, ensuring that patients receive coordinated care tailored to their specific conditions. Additionally, an emphasis on patient education and informed consent is crucial, empowering individuals to take an active role in their treatment journeys.
As the field of oral and maxillofacial surgery evolves, it remains essential for practitioners to stay abreast of these advancements to provide the highest standard of care. The combination of advanced techniques, digital innovations, and comprehensive patient engagement signifies a promising future, ensuring that oral and maxillofacial surgery can continue to meet the ever-changing needs of patients.
Conclusion
Oral and maxillofacial surgery is a vital field in healthcare, specializing in the diagnosis and treatment of conditions affecting the mouth, jaw, and face. This comprehensive guide has highlighted the multifaceted roles that oral and maxillofacial surgeons play in enhancing patient outcomes. One of the most significant aspects of this specialty is its ability to address complex health issues caused by oral diseases, traumatic injuries, or congenital anomalies. Left untreated, these conditions can lead to debilitating consequences that greatly impact quality of life.
We have discussed key surgical procedures such as tooth extractions, corrective jaw surgery, and facial reconstructive surgery—each integral to restoring both functionality and aesthetics. With advancements in surgical techniques and anesthesia, today’s procedures are safer, less invasive, and associated with faster recovery times.
Equally important is the interdisciplinary collaboration between oral and maxillofacial surgeons and other healthcare professionals. This approach ensures that patients receive comprehensive care that addresses not only physical challenges but also the psychological and social aspects of oral and facial conditions.
In this context, the clinic of Dr. Abdurrahman Ozturk in Istanbul stands out as one of the leading centers in Turkey for oral and maxillofacial surgery. With a commitment to innovation, patient safety, and individualized care, the clinic provides exceptional outcomes for both local and international patients.
Ultimately, the value of oral and maxillofacial surgery transcends individual procedures; it contributes to maintaining health, alleviating pain, and enhancing life quality. As awareness of this specialty grows, individuals are encouraged to seek timely care and benefit from the expertise of trusted professionals such as Dr. Abdurrahman Ozturk’s clinic, fostering a healthier and more informed society.