Introduction to Dental Implants
Dental implants represent a revolutionary advancement in modern dentistry, providing a durable and effective solution for individuals suffering from tooth loss. Essentially, a dental implant consists of a titanium post that is surgically placed into the jawbone, serving as a robust anchor for artificial teeth. This biocompatible material allows the implant to fuse with the bone through a process known as osseointegration, resulting in a stable foundation that mimics the function of natural tooth roots.
The significance of dental implants in contemporary dental practice cannot be overstated. They have emerged as a preferred option for tooth replacement, owing to their ability to restore not just the aesthetic appearance of a patient’s smile but also their functional capabilities. Unlike traditional methods such as dentures and bridges, which can lead to bone loss and require frequent adjustments, dental implants provide long-term stability. They also help maintain the integrity of the jawbone, stimulating bone growth and preventing the facial structure from collapsing.
Key benefits of dental implants include improved oral health, as they facilitate easier cleaning and care compared to removable dentures. Patients with implants tend to enjoy better chewing efficiency and overall comfort, significantly enhancing their quality of life. Research indicates that dental implants can last for many years, often a lifetime, with proper care, making them an economically sensible choice in the long run. The success rate for dental implants typically exceeds 95%, underscoring their reliability as a restorative option.
Overall, dental implants represent a pivotal innovation in dentistry, allowing individuals to regain functionality and confidence following tooth loss. Whether considering this option for cosmetic reasons or to improve oral health, understanding the fundamentals of dental implants is essential for making informed decisions.
Types of Dental Implants
Dental implants have revolutionized restorative dentistry, with various types designed to meet diverse patient needs. Among these, the most common are endosteal implants, subperiosteal implants, and zygomatic implants. Each type possesses distinct characteristics, suitable candidates, and specific applications.
Endosteal implants are the most widely used form of dental implants. These implants are typically made from titanium and are surgically placed directly into the jawbone. Ideal candidates for endosteal implants are individuals with sufficient jawbone density and volume, making them suitable for those who have lost teeth due to various reasons like periodontal disease or injury. Their success rate is high, often exceeding 95%, provided that the implant is placed by a skilled professional and adequate aftercare is maintained.
On the other hand, subperiosteal implants serve as a great alternative for patients who do not have enough healthy jawbone to support endosteal implants. This type involves placing a metal framework onto the jawbone under the gum tissue. As the gums heal, the framework becomes integrated with the bone. Subperiosteal implants are generally recommended for patients who are unable or unwilling to undergo bone augmentation procedures. Their application is less common than endosteal implants but remains an effective solution for specific dental implant cases.
Lastly, zygomatic implants are specialized dental implants that are anchored in the cheekbone (zygomatic bone) rather than the jawbone. They are utilized primarily in cases where severe bone loss has occurred in the upper jaw and a conventional dental implant would be inadequate. Suitable candidates for zygomatic implants may include individuals who have experienced significant bone resorption and those seeking immediate reconstruction after tooth loss. Overall, understanding these different types of dental implants allows patients to make informed decisions based on their unique dental needs and conditions.
The Dental Implant Procedure: Step-by-Step Guide
The dental implant procedure is a multi-step process that typically unfolds over several months, ensuring a thorough approach to restoring a missing tooth or teeth. The journey begins with a pre-operative consultation, where the dental professional conducts a comprehensive examination, including diagnostic imaging such as X-rays or CT scans. This assessment is vital for determining the patient’s oral health, bone density, and overall suitability for dental implants. During this consultation, various treatment options may be discussed, along with the potential benefits and risks associated with the procedure.
Once the preliminary evaluation is completed and a treatment plan is established, the next step involves the surgical placement of the dental implant. This is generally performed under local anesthesia, often complemented by sedation to ensure patient comfort. The dentist will make a small incision in the gum to expose the bone, creating a site for the implant. The titanium post is then inserted into the jawbone, serving as an artificial root. After placement, stitches are used to close the incision, and the healing process commences. This initial healing period, known as osseointegration, typically lasts from three to six months, allowing the bone to fuse with the titanium implant, ensuring its stability.
During the healing phase, patients may experience some discomfort, for which pain management strategies will be discussed, including over-the-counter pain relievers and prescribed medications as needed. Regular follow-up appointments are essential to monitor the healing and to ensure the implant is integrating properly. Once healing is sufficiently complete, a second procedure may be necessary to place a small connector piece known as an abutment. Following this, a custom-made crown or bridge will be crafted and securely affixed to restore function and aesthetic appeal, completing the dental implant procedure.
Who is a Good Candidate for Dental Implants?
Dental implants serve as a viable solution for individuals seeking to replace missing teeth, but not everyone may qualify as a good candidate for this procedure. Several factors play a pivotal role in determining eligibility for dental implants, beginning with a patient’s oral health. Individuals must possess healthy gums and sufficient bone density to support the implant. If bone loss has occurred due to periodontal disease or tooth loss, a bone graft may be necessary prior to the implantation.
Another crucial consideration is age. While there is no strict upper age limit for dental implants, candidates should be at least in their late teens or early twenties, when jawbone growth is typically complete. This ensures that the implants will integrate effectively with the jawbone over time. It is also important to note that younger candidates may be advised to wait until they reach full maturity, as their jaws may still be developing.
Overall medical conditions also influence a patient’s candidacy for dental implants. Conditions such as uncontrolled diabetes, blood clotting disorders, and autoimmune diseases can impede healing and increase the risk of complications. Moreover, individuals undergoing certain treatments, such as chemotherapy or radiation therapy, may face additional challenges. Thus, it is essential for candidates to disclose their complete medical history during consultations with dental professionals.
A thorough consultation with a qualified dentist or oral surgeon is imperative to assess one’s suitability for dental implants comprehensively. This process frequently includes X-rays and other imaging techniques to evaluate bone structure and the underlying anatomy. After a detailed analysis, the dental professional can provide tailored recommendations. Candidates who understand these crucial factors stand a better chance of successful implant procedures, ensuring enhanced outcomes and satisfaction.
Risks and Complications Associated with Dental Implants
Dental implant surgery, while generally considered safe and effective, is not without its potential risks and complications. Understanding these risks is crucial for anyone contemplating this procedure. One of the most common postoperative issues is infection at the implant site. This can lead to inflammation and pain, and in severe cases, it may result in implant failure. Bacteria can enter the area during or after surgery, making it essential for patients to maintain excellent oral hygiene and follow their dentist’s aftercare instructions diligently.
Another significant concern is implant failure, which occurs when the implant does not properly integrate with the surrounding bone. Various factors can contribute to this, including the patient’s overall health, the quality of the bone, and tobacco use. People with uncontrolled diabetes or those who smoke are at a greater risk, as these conditions can hinder healing and increase the likelihood of failure.
Nerve damage is also a potential complication of dental implant surgery. During placement, the implant may inadvertently contact nearby nerves, leading to sensations of tingling, pain, or numbness in the lips, gums, or chin. While nerve damage is rare, it can have long-lasting effects on a patient’s quality of life. Hence, selecting an experienced oral surgeon who utilizes advanced imaging techniques to plan the surgery can mitigate this risk.
Furthermore, proper aftercare and attending follow-up visits are critical elements in minimizing these risks. Patients should adhere to all the post-operative guidelines provided by their dentist, which may include dietary restrictions, modifications to oral hygiene routines, and the use of prescribed medications. By proactively managing these factors, individuals can significantly reduce the chance of complications, ensuring a successful outcome for their dental implant procedure.
Aftercare and Maintenance of Dental Implants
After the dental implant procedure, proper aftercare and maintenance are crucial for ensuring the longevity and vitality of the implants. One of the fundamental aspects of post-operative care is maintaining excellent oral hygiene. Patients should brush their teeth at least twice daily with a soft-bristled toothbrush, paying close attention to the implant site. Flossing is equally important, and using specialized tools such as interdental brushes or a water flosser can help clean hard-to-reach areas around the implant.
During the initial healing phase, patients should follow dietary recommendations to support recovery and optimize the success of the dental implants. Soft foods are encouraged in the early days following the procedure, as they pose less risk of disturbing the implant site. Foods like yogurt, mashed potatoes, and smoothies provide nourishment without requiring excessive chewing. As healing progresses, patients can gradually reintroduce firmer foods while still avoiding very hard items that could jeopardize the integrity of the implants.
In addition to at-home care, regular dental check-ups are paramount in maintaining the health of dental implants. It is recommended that patients visit their dentist every six months for professional cleanings and evaluations. During these visits, the dentist can assess the condition of the implants, check for any signs of infection, and provide necessary adjustments or treatments. These routine appointments play a critical role in preventing complications such as peri-implantitis, an inflammatory condition affecting the tissues around dental implants.
In conclusion, the aftercare and maintenance of dental implants involve diligent oral hygiene practices, careful dietary choices, and routine dental visits. By adhering to these guidelines, patients can help ensure the long-term success of their implants and enjoy their benefits for years to come.
Comparing the Cost of Dental Implants to Other Tooth Replacement Options
When considering tooth replacement options, understanding the financial implications is essential. Dental implants emerge as a preferred choice for many patients due to their longevity and functionality, yet they carry a higher initial cost compared to traditional replacements such as dentures and bridges. Generally, the average cost of dental implants can range from $3,000 to $4,500 per implant, which includes the surgical procedure, implant device, and the crown. In contrast, the total cost of dentures typically varies between $300 and $5,000, depending on the type and customization level chosen. Bridges can also range from $2,000 to $7,000, primarily influenced by the number of teeth being replaced.
While upfront expenses are critical to consider, examining the long-term financial aspects reveals a more nuanced picture. Dental implants may require a higher initial investment; however, they are considered a more enduring solution. Unlike dentures, which may need to be replaced or relined periodically, implants can last a lifetime with proper care. Their durability reduces the frequency and cost of replacements in the long run.
Furthermore, maintenance costs should also be factored into the overall financial evaluation. Dentures may necessitate regular adjustments and cleaning solutions, leading to ongoing expenses. Bridges, while often less costly than implants upfront, can incur future costs due to potential complications or the need for additional dental work if adjacent teeth are affected. Thus, while dental implants present a higher cost initially, their long-term stability and reduced maintenance needs can result in a more economical choice over time.
In conclusion, while the cost of dental implants may initially appear daunting, their relative durability and minimal maintenance make them a compelling option when compared to other tooth replacement solutions. By assessing both initial and ongoing financial obligations, patients can make informed decisions that align with their long-term oral health goals.
Latest Innovations in Dental Implant Technology
The field of dental implantology has witnessed remarkable advancements in recent years, significantly enhancing patient care and outcomes. One of the key innovations is the introduction of mini dental implants, which are smaller and require less invasive procedures than traditional implants. These mini implants are particularly beneficial for patients with limited bone structure, as they can be placed without the need for extensive bone grafting. This not only reduces surgery time but also accelerates recovery, making dental restoration more accessible to a broader range of patients.
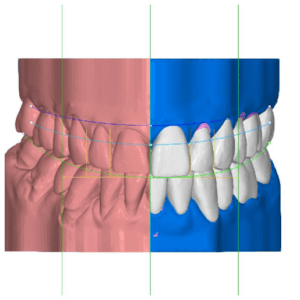
In addition to mini implants, computer-guided surgery has revolutionized the precision of dental implant placements. Utilizing advanced imaging techniques such as Cone Beam Computed Tomography (CBCT), dentists can create detailed 3D models of a patient’s mouth. This allows for meticulous planning and simulation of the placement procedure, improving accuracy and ensuring optimal positioning of the implants. As a result, computer-guided implants have been shown to reduce the risk of complications and enhance the overall success rate of dental procedures.
Moreover, advancements in materials science have led to the development of stronger and more biocompatible materials for dental implants. Titanium, previously the market leader, is now being complemented by innovative alternatives such as zirconia. Zirconia implants offer excellent aesthetics due to their natural tooth-like color, making them particularly appealing for patients seeking cosmetic solutions. Furthermore, new surface treatments are being explored to improve osseointegration, the process by which implants bond with the jawbone, thus enhancing durability and success rates.
These innovations have far-reaching implications for the future of dental implantology. With continued research and development, it is likely that patient experiences will improve, while the potential for complications and recovery times will lessen. The expansion of options in both materials and techniques signifies a promising horizon for dental implants, ultimately benefiting those seeking restorative dental solutions.
Patient Testimonials and Success Stories
Dental implants have transformed the lives of countless individuals, providing them with a renewed sense of confidence and improved oral health. Many patients have shared their testimonials regarding the transformative experiences they had while undergoing dental implant procedures. One such individual, Sarah, a 45-year-old teacher, had struggled with missing teeth for years. The embarrassment of her smile kept her from engaging in social situations. Upon receiving dental implants, Sarah noted a significant boost in her self-esteem: “I can finally smile without feeling self-conscious. It has made a huge difference in my overall happiness and confidence.”
Another inspiring story comes from John, a retired engineer in his late 60s. After losing multiple teeth due to decay, John faced difficulties in eating and drinking. The discomfort led him to avoid social events where food was involved. After consulting with his dentist, he decided to pursue dental implants. John recalls, “The procedure was straightforward, and the recovery was quicker than I expected. Now, I can enjoy meals with my family again without any discomfort.” His experience illustrates how dental implants can significantly enhance quality of life.
Moreover, testimonials often highlight the importance of the support provided by dental professionals throughout the process. Many patients, like Emily, have expressed gratitude for the guidance and care received during their journey. Emily states, “My dentist was incredibly thorough in explaining each step. They made sure I felt comfortable and informed.” Her positive experience underscores the value of professional care in successfully adapting to dental implants.
These real-life stories serve to inspire others who may be considering dental implants. They illustrate the challenges that can arise but ultimately emphasize the potential for remarkable transformation in health and happiness. With a blend of professional expertise and personal commitment, dental implants can pave the way toward a fulfilling life.












One Response