What Are Dental Implants?
Dental implants are advanced prosthetic devices designed to replace missing teeth, providing a long-lasting solution for individuals facing tooth loss. These implants are composed of several essential components that work collaboratively to mimic the natural structure and function of teeth. The primary material used in dental implants is titanium, renowned for its biocompatibility and strength. This remarkable metal facilitates a process known as osseointegration, in which the titanium post integrates with the jawbone, providing a secure foundation for artificial teeth.
At the core of a dental implant is the titanium post, which serves as a substitute for the tooth root. This post is surgically placed into the jawbone, after which it fuses with the bone over time, creating a stable base. The integration of the post into the bone is critical, as it ensures the durability and longevity of the dental implant. Once the healing process is complete, an abutment is attached to the titanium post. The abutment acts as a connector, protruding above the gum line to hold the custom-made crown in place.
The crown, typically crafted from porcelain or ceramic, is the visible part of the dental implant and is designed to closely resemble the appearance and function of natural teeth. Dentists focus on achieving a seamless match in color, size, and shape to ensure aesthetic harmony with the patient’s existing teeth. Together, the titanium post, abutment, and crown form a complete dental implant system that successfully restores dental functionality and enhances the smile’s appearance.
In essence, dental implants provide an effective and reliable solution for individuals requiring tooth replacement, allowing them to regain confidence in their smile and improve their overall oral health.
The Benefits of Dental Implants
When considering tooth replacement options, dental implants offer numerous advantages compared to more traditional choices such as dentures or bridges. One of the foremost benefits is the improved appearance that dental implants provide. These artificial teeth are designed to look and feel like natural ones, allowing individuals to regain their confidence and aesthetic appeal. The custom-made implants are tailored to blend seamlessly with existing teeth, ensuring a naturally attractive smile.
In addition to aesthetics, dental implants enhance comfort and functionality. Unlike dentures, which can sometimes slip or cause irritation, implants are securely anchored into the jawbone. This stability allows for ease of eating and speaking, enabling patients to enjoy their favorite foods without concern. Patients often report a significant improvement in their quality of life, as they no longer have to navigate the inconveniences associated with removable prosthetics.
Another critical benefit is the long-term durability associated with dental implants. With proper care, these implants can last many years, often a lifetime. This longevity makes them a cost-effective solution when considering the potential replacements and maintenance required for other options like bridges or dentures. Additionally, dental implants contribute to the preservation of jawbone health. When a tooth is lost, the jawbone can deteriorate over time due to lack of stimulation. Dental implants mimic the natural tooth root, thereby promoting healthy bone density and preventing further bone loss.
Overall, the benefits of dental implants are extensive, from enhancing appearance and comfort to ensuring durability and supporting oral health. These factors make implants a compelling choice for those seeking a reliable and effective solution to tooth loss.
The Dental Implant Procedure Explained
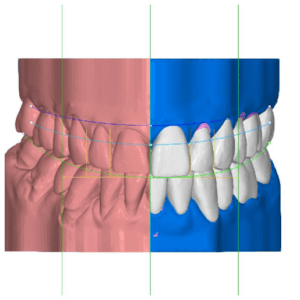
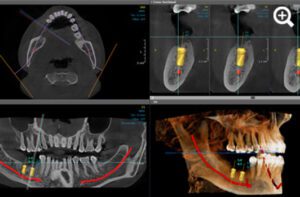
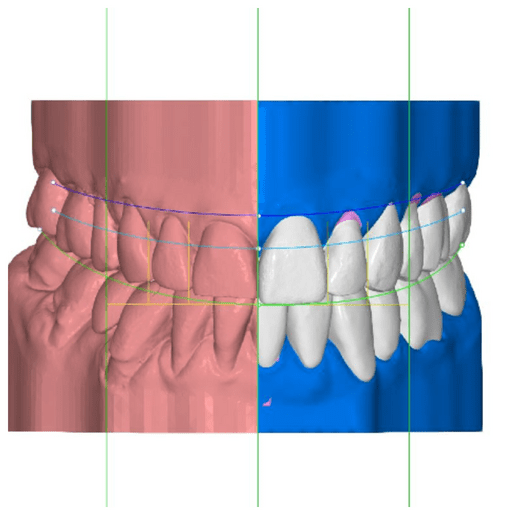
The dental implant procedure is a multi-step process designed to provide a durable and aesthetic solution for tooth loss. This procedure begins with an initial consultation, during which the dentist evaluates the patient’s oral health through a thorough examination, including imaging techniques such as X-rays or CT scans. During this assessment, the dentist will assess bone density and structure to determine if the patient is a suitable candidate for dental implants.
Once the suitability of the patient is confirmed, the next phase involves the surgical placement of the implant. This usually occurs in a clinical setting and requires local anesthesia to ensure the patient’s comfort. The dentist will make a small incision in the gum tissue to expose the bone. A titanium post, which acts as the artificial tooth root, will be carefully placed into the jawbone. Once securely positioned, the gum tissue is stitched back, covering the implant. At this point, the healing process begins, which can take several months as the bone integrates with the titanium post through a process known as osseointegration.
After adequate healing and successful integration of the implant, the next step is the attachment of the abutment—the connector piece that will hold the crown. This involves a minor surgical procedure where the gum is reopened to place the abutment, which will later be covered by the crown. Following this, impressions of the mouth are taken to create a custom crown that matches the surrounding teeth. The final appointment includes the placement of this crown on the abutment, completing the dental implant procedure.
Post-operative care is critical for successful healing and long-term implant success. Patients are advised on proper oral hygiene practices and may be prescribed pain management medications. Regular follow-up visits will ensure the implant remains healthy and functional.
Who Is a Candidate for Dental Implants?
Dental implants have gained popularity as an effective long-term solution for individuals who have lost teeth due to injury, decay, or other reasons. However, not everyone is an ideal candidate for this procedure. Several factors play a critical role in determining suitability, primarily focusing on oral health, bone density, and age.
First and foremost, having healthy gums is essential for anyone considering dental implants. Gums support the implant and play a significant role in the overall integration process. Gum disease or conditions that weaken the gum tissue can lead to complications and increase the risk of implant failure. Therefore, patients should be evaluated for any signs of periodontal disease prior to the procedure to ensure they have the right gum health to support an implant.
Another crucial factor is the presence of adequate bone density. Dental implants require sufficient bone to anchor securely within the jaw. If a patient has experienced significant bone loss, which can result from prolonged tooth loss or other conditions, additional procedures like bone grafting may be necessary before considering implants. A comprehensive evaluation through imaging technologies, such as X-rays or 3D scans, helps in determining bone density and overall jaw condition.
Age also influences candidacy for dental implants, though there is no strict age limit. Generally, individuals must have completed jawbone development, which typically occurs by the late teens to early twenties. However, older adults can also benefit from implants, provided they maintain good oral and overall health.
Lastly, existing medical conditions can impact eligibility. Certain health issues, such as uncontrolled diabetes or autoimmune diseases, may interfere with healing and increase the risk of complications. A thorough medical evaluation is vital in assessing a patient’s overall health status and identifying potential contraindications to ensure the best outcomes for dental implant procedures.
Recovery and Aftercare for Dental Implants
Following dental implant surgery, patients may experience a range of sensations and symptoms as part of the healing process. Initially, it is common to feel discomfort and soreness in the surgical area. This post-operative discomfort can usually be managed effectively with prescribed pain medications or over-the-counter pain relievers. Additionally, applying ice packs to the affected area for short intervals may help reduce swelling, which is a normal part of the body’s response to surgery.
In terms of healing, the dental implant procedure typically requires a recovery period of several days, during which patients should be mindful of their oral hygiene practices. It is crucial to avoid vigorous rinsing or spitting within the first 24 hours after surgery, as this can dislodge the blood clot that is vital for healing. Gentle brushing can be resumed on the day after surgery, but care should be taken to avoid the implant site until it is fully healed. The precise recovery timeline can vary from person to person, usually taking anywhere from a few weeks to several months for the implant to integrate properly into the jawbone.
During the first few days, patients are advised to maintain a soft-food diet to prevent any undue pressure on the healing gums. Foods such as yogurt, mashed potatoes, and smoothies can provide nutrition without irritating the surgical site. It is prudent to stay hydrated as well, avoiding straws that can create suction and potentially hinder the recovery process. Regular follow-up visits with the dental specialist are necessary to monitor healing and assess the success of the implant integration.
Overall, adhering to the recommended aftercare practices plays a significant role in ensuring the best outcomes for dental implants. By being proactive about pain management, maintaining good oral hygiene, and attending follow-up appointments, patients can support their recovery and promote successful implant integration into their dental anatomy.
Potential Risks and Complications
Dental implant surgery is generally considered a safe and effective procedure for replacing missing teeth. However, as with any surgical intervention, there are potential risks and complications that patients should be aware of prior to undergoing the treatment. Understanding these risks is essential in making an informed decision about whether dental implants are the right choice for you.
One of the primary risks associated with dental implants is infection. This can occur at the surgical site, leading to inflammation and complications that could jeopardize the healing process. Proper oral hygiene and following post-operative care instructions provided by your dental professional are crucial in minimizing the risk of infection.
Another potential complication is nerve damage, which may occur during the placement of the implant. This can result in persistent pain, tingling, or numbness in nearby areas such as the gums or lips. It is important for your dental surgeon to thoroughly assess the anatomy of your jawbone and surrounding structures to mitigate this risk.
Implant failure is also a possibility, which may occur due to inadequate bone integration or insufficient support from the jawbone. Several factors may contribute to this issue, including pre-existing medical conditions such as diabetes or osteoporosis, as well as lifestyle choices like smoking. Discussing these risk factors with your dentist can help ensure a higher success rate for your dental implants.
Additionally, sinus issues may arise particularly when upper jaw implants are placed. The implant may protrude into the sinus cavity, causing discomfort or leading to sinus infections. Thorough pre-surgical evaluations and imaging can identify potential anatomical concerns and guide the planning for implant placement.
In conclusion, while dental implants can enhance oral functionality and aesthetics, it is essential to be aware of the associated risks and complications. Open communication with your dental professional will help you navigate these potential challenges and make the best decision for your oral health.
Cost Considerations of Dental Implants
The financial aspect of dental implants is a significant concern for many individuals considering this option for tooth replacement. The overall cost of dental implants can vary widely based on several factors. The complexity of the procedure, the type of materials used, the location of the dental clinic, and the expertise of the dental professional all play a role in determining the final price. On average, dental implants can range from $3,000 to $4,500 per implant, excluding any additional procedures such as bone grafting or sinus lifts that may be necessary for successful placement.
There are also varying costs associated with the dental implant components. For example, the titanium implant itself, the abutment, and the crown can incur separate charges. This modular pricing structure can make it difficult for patients to estimate the total financial commitment upfront. As part of a comprehensive cost analysis, individuals should also consider post-operative care, which may require follow-up visits or additional treatments, further impacting the overall expenditure.
Insurance coverage for dental implants can also influence the financial burden on patients. While some insurance plans may cover a portion of the implant procedure, others may classify it as a cosmetic treatment and exclude it altogether. Therefore, it is imperative for patients to review their insurance policies carefully and consult with their providers to understand their specific coverage options.
For those who may face financial constraints, several financing options are available. Many dental clinics offer payment plans, allowing patients to spread the cost over several months. Furthermore, third-party financing solutions like CareCredit provide accessible payment alternatives, allowing for manageable monthly payments. Understanding these cost considerations can help patients make informed decisions regarding their dental health and potential investment in dental implants.
Comparative Analysis of Dental Implants
When considering tooth replacement options, patients often evaluate several alternatives, such as dental implants, dentures, and bridges. Each of these solutions has distinct strengths and weaknesses that cater to varying needs and circumstances.
Dental implants are widely recognized for their durability, aesthetic appeal, and functionality. They integrate with the jawbone, providing stability akin to that of natural teeth. This biological integration helps prevent bone loss, a common consequence of tooth extraction. Furthermore, implants do not require alteration of adjacent teeth, preserving overall dental health. However, the placement of dental implants necessitates a surgical procedure, and candidates must have sufficient bone density, which may limit the option for some patients.
On the other hand, dentures are a more traditional solution for tooth loss and are generally less invasive. They can be removable or fixed, offering versatility to those who may not be candidates for implants. Dentures can restore function and appearance relatively quickly and are often more affordable upfront. However, they may cause discomfort and require adjustments over time. Patients may experience challenges with denture stability, leading to difficulties in chewing and speaking.
Bridges provide another viable alternative, especially for those who are unable or unwilling to undergo surgical procedures. They involve anchoring artificial teeth to adjacent natural teeth. Bridges restore function and aesthetics effectively, but they do require the modification of surrounding teeth, which can compromise their long-term health. Additionally, they do not address the risk of bone loss, as they do not stimulate the jawbone like implants do.
Ultimately, the choice between dental implants, dentures, and bridges should be guided by individual health conditions, lifestyle preferences, and budget considerations. Assessing these options thoroughly can help patients make informed decisions regarding their dental care and overall oral health.
Maintaining Your Dental Implants
Maintaining dental implants is essential to ensure their longevity and function. Proper care extends beyond the initial placement and requires diligent effort from the patient. Daily oral hygiene practices play a pivotal role in the maintenance of dental implants. Just as one would care for natural teeth, it is crucial to brush and floss around the implants regularly. Using a soft-bristled toothbrush and non-abrasive toothpaste will prevent damage to the implant surface. Additionally, special floss or interdental brushes designed for dental implants can be used to clean areas that are often difficult to reach, thereby reducing plaque accumulation.
Routine dental check-ups are equally important in the ongoing care of dental implants. These appointments allow for professional cleaning, thorough examinations, and timely identification of potential issues. During these visits, a dentist can assess the health of the gums surrounding the implant and ensure that there are no signs of peri-implantitis, an infection that can threaten the stability of the implant. Regular check-ups typically occur every six months, but some patients may require more frequent visits based on individual circumstances.
In addition to oral hygiene and professional care, lifestyle choices significantly impact the longevity of dental implants. Avoiding harmful habits, such as smoking, can enhance implant success rates. Smoking not only hinders healing but also increases the risk of gum disease, thereby jeopardizing the integrity of the implants. Furthermore, adopting a balanced diet rich in vitamins and minerals can promote gum health and overall oral well-being. In conclusion, maintaining dental implants requires a commitment to diligent oral hygiene, regular dental visits, and healthy lifestyle choices. By emphasizing these aspects, patients can maximize the benefits of their dental implants and maintain a healthy smile for years to come.